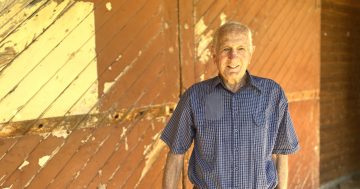
Australians are getting older and living longer, but are we doing enough to plan for it? Photo: wirestock.
In between taxes and death, there’s another certainty in life – ageing. It happens to all of us, although some certainly do it better than others.
When we’re young we think our parents are old. Then we become parents and don’t feel old at all. We go from worrying about our kids to worrying about our parents.
So in a country that is rapidly ageing, why aren’t we talking more about it? Why aren’t we better at making plans for our old age and for looking after our ageing communities?
By 2050, according to the Australian Human Rights Commission, about one quarter of all Australians will be aged 65 years and over. By then, it’s estimated that 1.8 million Aussies will be aged 85 and over.
It’s almost ironic that we are forever bombarded with messaging about living healthier – don’t smoke, limit alcohol intake (but red wine is OK), do more exercise, eat more fruit and veggies, eat meat/don’t eat meat, get more sunshine but not too much – all in the name of living longer.
So now that we’re living longer – and healthier to boot – what does that mean to our society as a whole?
An ageing community needs more support, medically, physically and mentally. That means more health and community workers, more GPs and specialists, more research into dementia and other age-related illnesses.
As people age, they need housing security, whether that means help to remain in their own homes, or a move into an aged care facility – if an appropriate and affordable place can be found.
They need access to services and that starts with simply knowing what services are available. And if you’ve ever done battle with a bureaucracy you’ll know just how bloody difficult it can be to cut through the red tape to request those services.
My beautiful, intelligent, creative, talented mother is showing signs of early-onset Alzheimer’s.
She’s still more than capable of living on her own and driving to nearby familiar places, at least for now, but we can see it’s becoming harder, more frustrating for her and more worrying for the family.
Mum is of the generation of women who generally stayed home to raise the children (at least that’s what Dad wanted), but she had an extensive and varied career.
However, most of her working life was in an era before compulsory employer superannuation, so as an older, single woman she exists on the pension, reliant on subsidised housing.
As we’ve been doing the rounds of GPs, specialists and myriad tests on all parts of her mind and body, I’m just thankful that both my sister and I live close by so we are able to support Mum. Sometimes that includes financial support, especially when her pension just can’t stretch to cover up-front medical costs.
One of us now goes with her to all medical appointments because she has trouble retaining what she is told, or forgets to get pathology tests or scripts filled.
We are so grateful – Mum included – that she hasn’t lost her sense of humour. Driving her to the geriatrician one day, Mum asked where we were going. When I told her she asked, “And why am I seeing him?” We both cracked up when I told her it was for her memory issues.
Neither my sister nor I have a medical background so we take copious notes at every visit because we know it’s important that her GP, geriatrician and cardiologist, let alone the rheumatologist and all the other “ists”, are kept in the loop with every test result or new medication. And our brains need a reminder too.
We both work full-time but generally have the flexibility to allow us time to be with Mum – even when a 15-minute GP visit actually takes more than an hour in the waiting room.
But what happens to older people who don’t have that family support? Who need more specialist care but don’t know how to get it, or even who to ask? Who are physically healthy but failing mentally? Who end up “trapped” in a hospital bed because it’s not safe for them to live on their own anymore?
Region recently published a story on a novel program started by the Community Industry Group to help elderly people stuck in hospital beds to transition into more suitable living arrangements at home or in a residential aged care service.
The patient’s original reason for coming to hospital may well have been resolved, but because they can’t be safely released, they’re stuck in hospital – in some cases for more than 200 days.
The Supported Transition Assistance Response Scheme program involves volunteers who will provide personalised assistance to the older person to navigate their way out of hospital, explore suitable aged care and service options and give the patient confidence in their decision-making.
Obviously it also helps to clear beds for incoming patients which in turn helps to reduce waiting times in emergency departments – a win-win all round.
But more importantly, it hands dignity and control back to the patient.
They say it takes a village to raise a child; today and into the future I think the village will need to come together to help us age.
Original Article published by Jen White on Region Illawarra.