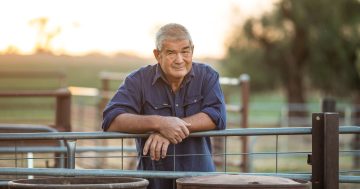
Dr Peter Baldwin, head of clinical research at the Black Dog Institute, wants Eurobodalla people to safeguard their mental health.
Areas such as the Eurobodalla, which was ravaged by bushfires in the year leading up to the global pandemic, are high risk for people experiencing mental health problems.
That’s the message from Dr Peter Baldwin, head of clinical research at the Black Dog Institute.
According to Dr Baldwin, the mental health problems of people in regional and rural areas have been further exacerbated by pre-existing risk factors such as isolation and a lack of access to mental health care.
“There’s a lot less specialist services – people like psychiatrists and clinical psychologists,” he said.
“People who are trained to deal with the more complex presentations are even harder to get to, so when these mental health challenges present themselves it becomes much more difficult to address them.”
For Eurobodalla people with mental health problems, pandemic isolation and trauma from the bushfires haven’t helped.
“Being connected with other people and being supported is a really strong protective factor in mental health,” Dr Baldwin said.
“Without that, we all tend to suffer a little bit more.”
Dr Baldwin said it became a vicious cycle when you added to that a pre-existing lack of access to mental health care.
“People tend to get worse without treatment, and then end up in a more severe state, requiring more complicated care, which again they can’t access,” he said.
Dr Baldwin said concerning risk factors for mental health, such as drug and alcohol misuse, were more prevalent in regional and remote areas.
“We already knew that people in regional and remote areas were more likely to use those sorts of things to cope with mental health problems – probably largely because they couldn’t access anything else,” he said.
Dr Baldwin urged people living in regional and remote areas to take action and safeguard their mental health.
“One of the good things about the adoption of video technology is we can use it for social things as well,” he said.
“One thing that people can do is book something in and have it in the calendar regularly.”
Dr Baldwin encouraged people to attend regular stress check-in group meetings.
“A pandemic support group … where the purpose of the group is to talk about things that are stressing you,” he said.
The benefit of outlets such as these, according to Dr Baldwin, is that no one person carries the burden of the group.
“You can balance complaining with problem solving, where you get to have your rant and you get to feel heard, but you also access the wisdom of your community in terms of solving the problems,” he said.
“It can really ignite community action to solve problems (and) it helps turn pain into purpose.”
Dr Baldwin encouraged people to have some fun with it by handing out a prize to the person who has had the worst month.
“It can just add a little bit of levity to an otherwise pretty horrible situation,” he said.
“Also, it really does encourage sharing of difficult things and that’s really what … I know a lot of people in regional and remote areas struggle to do.
“Often communities are small and there’s a culture of stoicism … which is a strength and a weakness.”
Black Dog Institute is running a series of freely available webinars and presentations to try to bridge the gap between services and remote and rural areas.
“You can have someone come and speak to your community, in your community, about things like breaking down depression … and practical advice for dealing with it,” Dr Baldwin said.
“We also have webinars that are available … that people can access online if they prefer to do it in privacy or in their own time.”
The institute’s specialist telehealth services are also freely available, including a natural disaster support service for people who have been impacted by natural disasters such as bushfires.
“These services are delivered by expert clinical psychologists who have considerable training and experience in trauma,” Dr Baldwin said.
“For people who are experiencing real PTSD, getting specialist mental health care can be a challenge, and waiting lists are huge. With our natural disaster support service, people can come in and they can access an expert clinical psychologist for free.”
The institute has also built a mental health hub for health professionals.
“We’re working with two groups who generally are not the sort of people who rush to get mental health support: health professionals and people who live in regional areas,” Dr Baldwin said.
“Both cultures are really all about toughing it out, getting on with things, and perhaps mental health being stigmatised, so we’re seeing more and more as we build trust with those communities and groups, that people are accessing the service and people are getting real benefit from it.”